" introduction
Complications
The most severe complication of ulcerative colitis is toxic megacolon. It is a condition in which the colon becomes paralyzed, preventing any passage of gas or material; symptoms include fever, sweat, and weakness. If the condition is not treated, the colon can stretch to the point of rupture, which is quite dangerous for the individual's survival.
Additional complications of ulcerative colitis: as a consequence of the severe inflammatory state and persistent diarrhea, fever, dehydration, iron deficiency anemia, vitamin and mineral deficiencies, loss of strength and appetite, growth retardation may arise. Extraintestinal disorders such as arthritis, eye and skin lesions, liver and biliary tract diseases, ankylosing spondyloarthritis are also possible. Immunosuppressive drug therapy may also increase susceptibility to infectious diseases.
Patients with ulcerative colitis have an increased risk of developing colon cancer; nevertheless, more than 90% of them will not face the disease in their lifetime. The risk is greater for those patients in whom the inflammation extends to the entire colon and lasts for at least eight to ten years; in such conditions it is recommended to perform a colonoscopic examination every 12-24 months.
Treatment
For further information: Drugs for the treatment of Ulcerative Colitis "
The treatment, initially pharmacological, uses pain-relieving and anti-inflammatory drugs, which prevent complications in the acute phase and help the patient to control the symptoms in the chronic phase.
In cases that do not respond to medical therapies, or in the presence of neoplasms, partial or total surgical resection of the colon is used.
For further information: Colon resection - Colectomy "
Diet and Ulcerative Colitis
For further information: Diet and Ulcerative Colitis "
At present there is no definite evidence on the link between the consumption of certain foods and the onset of ulcerative colitis. Numerous theories have been proposed in this regard, but none have ever been confirmed and universally accepted. One of the first, just to cite a few examples, identified milk as the triggering element, especially for people who are allergic or intolerant to lactose. Chemical food additives have also been investigated for a long time, without however obtaining confirmation of the initial suspicions.
It is currently believed that a diet rich in calories, fat and sugar, but at the same time low in fiber, while not representing a certain etiological agent, can somehow favor the onset of the disease. Confirming this, the incidence of ulcerative colitis is significantly higher in the United States and England than in Asian and African countries, which points to the existence of a link between typically Western eating habits and disease.
There are also certain foods that can aggravate symptoms, particularly during acute inflammatory episodes. Dairy products, for example, can amplify intestinal disorders, especially if the patient is lactose intolerant. In the same way, too abundant meals and an excessive consumption of fibers could accentuate abdominal swelling and disorders of the hive. Finally, stress should be kept under control, since the continuous succession of stressful stimuli increases gastric acidity, interferes with normal intestinal transit and facilitates the exacerbation of ulcerative colitis.
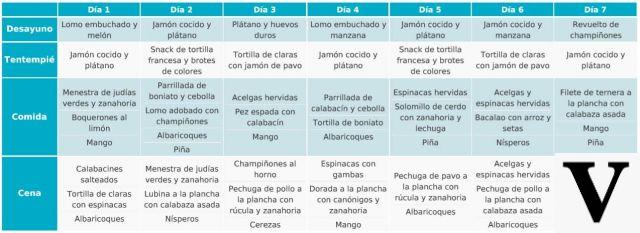
Diet and ulcerative colitis, some tips
- Abolish spices, spicy foods (pepper, chilli, curry, nutmeg), alcohol, carbonated drinks, tea (allowed decaffeinated), coffee (allowed decaffeinated) and chocolate.
- Reduce or even eliminate the consumption of milk; on the other hand, moderate quantities of yoghurt and dairy products are tolerated (with the exception of spicy cheeses). The consumption of probiotic foods may be useful, however, it will have to be evaluated by the doctor.
- Reduce the presence of meteoric foods, such as legumes, in your diet.
- Also moderate the consumption of fiber, preferring refined foods to wholemeal ones.
- Avoid fiber supplements and do not overdo the consumption of fruit (which must be peeled) and vegetables (which can be centrifuged, but not blended to keep the meteorism under control).
- Increase your consumption of fish and flax seeds, while reducing that of dried fruit and seed oils. In this way you will rebalance the ratio between omega-six and omega-three in your diet, taking full advantage of the beneficial anti-inflammatory action of the latter.
- In the presence of steatorrhea (excessive amount of fat in the stool), it is possible to resort to supplements of medium and short chain fatty acids (for example MCT oils), which are absorbed directly by the intestinal mucosa without undergoing any digestive process.
More articles on 'Ulcerative Colitis: Diet and Treatment'
- Ulcerative colitis
- Drugs for the treatment of Ulcerative Colitis
- Ulcerative Colitis - Herbal Medicine