The so-called "diet for pancreatitis" is a dietary strategy which, if necessary, favors the cure of the disease and opposes the deterioration of general health.
Pancreas, Pancreatitis and Diet
What is pancreatitis?
Pancreatitis is an inflammatory disease affecting the pancreas.
The pancreas can be considered both an organ and a gland; it is in fact responsible for the endocrine secretion of hormones (insulin, glucagon) and the exocrine secretion of a juice with digestive action (containing trypsinogen, chymotrypsinogen, elastase, pancreatic lipase, pancreatic amylase, pancreatic phospholipase and pancreatic nuclease).
By negatively affecting these functions of the pancreas, pancreatitis worsens the digestion of food and the metabolism of some nutrients; this explains the need to adopt a specially calibrated diet.
Causes and Consequences
The triggering causes of pancreatitis can be very varied, but they are all characterized by a kind of "self-digestion”Of the gland which, depending on where it is damaged, loses its typical secretory capacity.
When the pancreas is affected by an inflammatory process, the cells are damaged and its digestive enzymes come into contact with the surrounding tissues, degrading them to the point of causing hemorrhages, infections, etc; in the event that these digestive juices enter the bloodstream, very distant organs such as the kidneys and the heart may also be involved.
Purpose of the Pancreatitis Diet
It is therefore quite logical to think that the diet for pancreatitis is essential for improving the state of health and for a better prognosis.
These nutritional regimes are not aimed at removing the agent triggering the pathology but, on the other hand, they are very important for the restoration / maintenance of the nutritional condition, without which the body is hardly able to overcome a critical situation.
The diet for acute pancreatitis and the nutritional regimen for chronic pancreatitis are quite different.
After clarifying the differences between the two clinical pictures, we will analyze in more detail the guidelines to be followed.
Types of Pancreatitis
Pancreatitis is classified into two categories:
-
Acute pancreatitis: sudden onset and high danger of death; the most frequent causes are: pharmacological, traumatic, alcohol abuse and gallstones (if it obstructs the choledochus); more rarely, infectious or poisonous.
The main symptom of acute pancreatitis is pain (localized or radiated) but nausea, vomiting, fever and increased heart rate also appear. The diagnosis must take into account the presence of pancreatic enzymes in the blood, the increase in certain electrolytes and glucose.
Therapy (if necessary) is aimed at removing the triggering agent. Maintaining your country's parameters and compensating for complications are of great importance; sometimes, surgery is necessary (removal of cysts, stones, necrotic tissue, etc.). Mortality is estimated at 15%. -
Chronic pancreatitis: has an etiology frequently related to: alcohol abuse (70% of cases), autoimmunity, use of certain drugs and familiarity.
It occurs mainly following a failure or partial resolution of acute pancreatitis. In the long term, serious complications can arise such as: difficult to reverse weight loss, diabetes mellitus and digestive disorders.
The immediate symptom is pain (localized or radiated); later, clinical signs may appear that correspond to the complications themselves, namely nutritional malabsorption of various kinds (including weight loss) and, in an advanced stage, diabetes mellitus (which is also one of the most important complications).
Diagnosis can be made using systems such as blood analysis, ultrasound, computed tomography, etc.
The treatment is aimed at moderating pain and maintaining nutritional parameters, which is why a specific diet associated with the intake of drugs containing pancreatic enzymes becomes essential.
Mortality is lower than in the acute phase and appears to be mainly related to complications associated with certain comorbidities.
Acute pancreatitis diet
The diet for acute pancreatitis varies greatly based on the severity of the disease.
In the most severe forms, it is better to avoid any form of oral feeding, whether based on food or based on parenteral solutions (nasogastric tube).
This is absolutely necessary to keep the organ at rest which, in most cases, is unable to perform its endocrine function or its exocrine function adequately.
Nutrition for severe acute pancreatitis takes place mainly intravenously and is often associated with drugs of the type: analgesic, antibiotic, hormonal (insulin) etc.
The requirements of parenteral nutrition for severe acute pancreatitis are:
- High water content
- Concentration of carbohydrates proportional to glycaemia
- Low lipid content, mainly composed of medium-chain fatty acids
- Medium portion of essential amino acids
- Salts and vitamins in normal quantities.
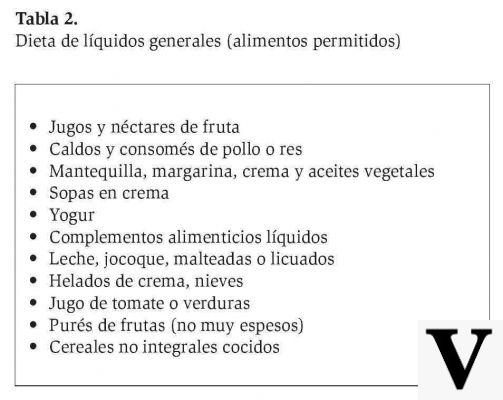
In the milder forms, however, when the resolution is estimated in approximately 24 or 48 hours, it is possible to forego the intravenous nutritional administration by limiting the water compensation; in some cases, it is possible to start the food-based diet early.
For both situations, from the moment the pancreatic enzyme levels are back in the ordinary, it is possible to start with the solid diet.
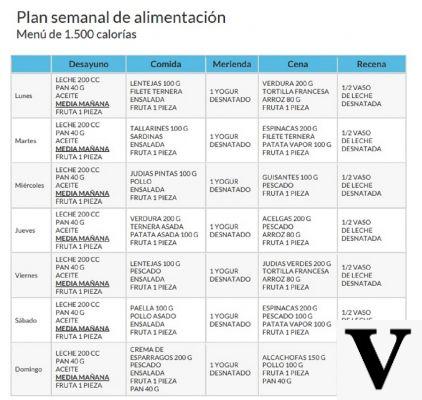
The basic requirements of this diet are:
- TOTAL elimination of alcohol (including wine with meals) and drinks with other nerves (coffee, tea, energy, etc.)
- High splitting of total energy, with at least 6 small meals
- High water content
- High carbohydrate content, especially with a low glycemic-insulin index
- Low concentration of carbohydrates with a high glycemic-insulin index (especially in the case of diabetes mellitus)
- Low lipid content
- Modest protein content of animal origin, to be progressively increased.
Chronic Pancreatitis Diet
Chronic pancreatitis is characterized by a state of chronic malabsorption (more or less severe), sometimes associated with dyspepsia and pain (which can increase with meals); this often causes the sick to refuse food.
The goals of the diet for pancreatitis are to counteract malnutrition due to malabsorption and to stimulate pancreatic activity to a minimum.
The basic requirements of this diet are:
- TOTAL elimination of alcohol (including wine with meals) and drinks with other nerves (coffee, tea, energy, etc.)
- High splitting of total energy, with at least 6 small meals
- High water content
- Normal concentration of carbohydrates, preferably with a low glycemic-insulin index; about 60% of the total energy
- Normal concentration of proteins; about 15% of the total energy or 0,8g per kg of desirable physiological weight
- Minimum concentration of lipids; about 25% of the total energy
- Amount of fiber equal to or less than 15-20g / day.
It is desirable, especially in cases of more pronounced malabsorption, the use of vitamin supplements. This intervention is necessary due to the poor digestive potential, in particular of the fat-soluble molecules (moreover, taken in limited quantities to avoid pancreatic fatigue).
Sometimes, doctors choose to give drugs containing pancreatic enzymes to compensate for the functional deficit.
The main sources of carbohydrates with a low glycemic-insulin index must be hulled legumes and refined cereals, preferably in soupy recipes. This recommendation, which does not seem to respect the need to moderate the glycemic-insulin index, is essential to avoid that the fibers excessively hinder the action of enzymes (both endogenous and exogenous).
High biological value proteins should be taken through the combination of legumes and cereals, and from lean foods of animal origin such as: chicken and turkey without skin, lean cuts of veal - beef, pork loin, sea bream, sea bass, cod, plaice, egg whites, low-fat cheese flakes (better to avoid other dairy products), etc.
The cooking of all foods must be totally free of added fats, which is why it is suggested to use non-stick pans or to practice techniques such as: boiling, steaming, pressure, bain marie, pot and vacuum.
In the diet for chronic pancreatitis, the seasonings should be based on oils rich in medium-chain fatty acids, the absorption of which is independent of the action of bile and pancreatic lipases; in principle, it is better not to exceed 30-40g / day.
The oil that boasts the greatest amount of medium-chain fatty acids is coconut oil; even butter boasts a fair percentage of it, but it is not recommended due to the saturated nature of the fatty acids that compose it.
Other articles on 'Pancreatitis Diet'
- Pancreatitis - Medicines for the treatment of pancreatitis
- Pancreatitis
- Pancreatitis: diagnosis, care and treatment