generality
Myelosuppression is a medical condition characterized by a reduced production of blood cells by the bone marrow.
Also known as myelosuppression or myelotoxicity, it is one of the most important side effects of chemotherapy treatments used for the treatment of tumors. Not all these drugs induce myelosuppression and the extent of the same depends - as well as on the type of drug - also on the doses, on the methods of administration, on the patient's health and on the number of previously administered administrations.
Immunosuppressive pharmacological treatments, used in case of autoimmune diseases (e.g. rheumatoid arthritis, Crohn's disease, scleroderma, lupus, etc.) or organ transplants can also cause myelosuppression. Very rarely, the condition is a side effect of long-term therapy with non-steroidal anti-inflammatory drugs or thiazide diuretics.
Parvovirus B19 targets red blood cell precursor cells, which it uses to replicate. Often asymptomatic, the infection can cause myelosuppression problems (especially anemia) in people with compromised bone marrow or immune function.
Particularly severe myelosuppression is called myeloablation.
Consequences
In individuals with myelosuppression, the bone marrow is unable to synthesize adequate amounts of blood cells.
The following table schematically shows the prevalent functions of blood cells and the consequences of their pathological reduction.
| Blood cell | Main functions | Consequences of a reduction |
| Erythrocytes (red blood cells) | Transport of oxygen in the blood | Feeling of physical exhaustion, shortness of breath, easy fatigue |
| Leukocytes (white blood cells) | Immune activity (prevent and fight infections) | Increased risk of infections, including severe ones |
| Platelets (piastrine) | Blood coagulation | Appearance of bruising and abnormal bleeding; increased risk of bleeding |
In general, the consequences of myelosuppression are all the more serious the more marked is the reduction of blood cells.
Of particular concern, in the oncological field, are the levels of white blood cells and especially of neutrophilic granulocytes; this is because their excessive decrease makes the patient susceptible to the development of a wide variety of potentially fatal infections.
Considering the dangers for the patient's survival, the use of drugs responsible for myelosuppression is contraindicated in case of:
- severe ongoing infections;
- severe impairment of bone marrow function;
- recent vaccination with any live vaccine (even if attenuated).
It should also be borne in mind that:
- bone marrow depression by myelotoxic drugs is usually dose related (increases with increasing dose of drug administered);
- multiple combinations of myelotoxic drugs can amplify myelosuppression by additive or synergistic effect;
- myelosuppression can be subject to cumulative effects of the same chemotherapy treatments; it means that it can get worse after repeated courses of drug treatment.
Myelosuppression for chemotherapy
Many chemotherapy drugs have negative effects on tissues characterized by a high rate of cell turnover, as occurs, for example, in the hair follicles, mucous membranes or blood.
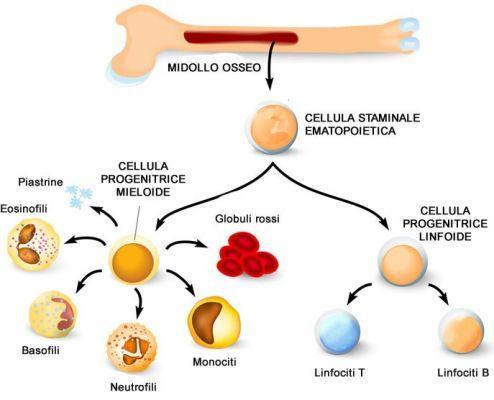
Blood cells, in particular, are synthesized in the bone marrow in a defined process hematopoiesis. This process begins with progenitor stem cells, which possess the ability to differentiate into the different hematopoietic lines that give rise to white blood cells, red blood cells and platelets respectively.
Chemotherapy drugs create damage to these progenitor cells, while in general they do not create significant damage to mature blood cells.
Since the average life of mature white blood cells is 12-16 hours, that of platelets is 10-24 days, and that of red blood cells is 100-130 days, the first effect of chemotherapy myelosuppression is white blood cell deficiency, while the shortage of red blood cells is the last to appear.
Treatment
In the case of severe myelosuppression, medical treatment is essential to try to restore normal blood cell levels. Among other things, the latter represent an important indicator for deciding when the patient can undergo a new course of immunosuppressive chemotherapy; this is because repeating the treatment when the blood values are still too low represents a serious danger to the patient's life.
The treatments of myelosuppression are different, as are the related purposes:
- broad-spectrum antibiotic prophylaxis and use of strategies and aids (washing hands, wearing masks, gloves, etc.), up to isolation in "sterile" rooms: this treatment aims to prevent serious infections of the neutropenic patient;
- administration of erythropoietin and erythropoietin analogues: they have the purpose of stimulating the synthesis of red blood cells, preventing anemia;
- administration of specific growth factors for certain subpopulations of white blood cells (e.g. filgrastim, lenograstim or pegfilgrastim);
- administration of interleukin-11: promotes the maturation of platelet precursors in the bone marrow;
- blood transfusions: transfusions of whole blood or of its individual components (for example platelets) may be necessary to limit the serious consequences related to myelosuppression.
Some of these treatments can also be carried out for preventive purposes.
The length of time it takes to reach the nadir (i.e. the lowest point of blood cell values over time), as well as the median time to normalization of blood values in the myelosuppressed patient, depend on the drug or drug combination and dosages. used. Generally speaking, it takes three to six weeks on average for a satisfactory recovery.
The onset of complications from myelosuppression, in addition to endangering the patient's life, compromises the effectiveness of the anticancer treatment; in fact, it can cause delays in subsequent cycles or a reduction in the dose of chemotherapy subsequently administered.