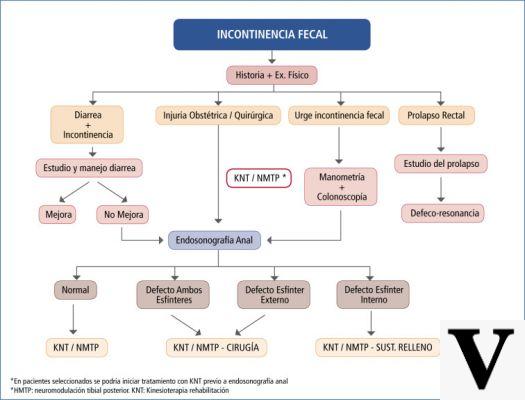
The problem of fecal incontinence
We speak of fecal incontinence when it is no longer possible to control or simply perceive the urge to defecate; the result is therefore an uncontrolled and involuntary emission of stools and intestinal gas.
Fortunately, fecal incontinence is not as incurable as one might assume. A specific medical treatment for attack, supported by a targeted and balanced diet, is undoubtedly the ideal solution to ward off this unpleasant disorder and prevent complications and relapses.
To definitively cure faecal incontinence it is necessary - as well as indispensable - to act on several fronts:
- Eradicate the cause that induced it: to find the right cure it is therefore important to undergo all the diagnostic tests necessary for the correct evaluation of the disorder
- Correct improper eating habits
- Take care of your body: for this purpose, personal intimate hygiene plays a leading role
- Always discuss any concerns and concerns with your doctor, especially if you have any abnormal or suspicious symptoms / signs
There is no universal cure to combat fecal incontinence because the disorder has a multifactorial origin. In fact, while some patients require surgery, for others it is sufficient to change their eating habits and follow an exclusively pharmacological treatment.
Pharmacological treatment
Pharmacological treatment for fecal incontinence is also not the same for all patients. As we have seen, in fact, this defecation disorder can depend on completely different or even opposite problems (eg chronic constipation or chronic diarrhea).
- Case 1: fecal incontinence dependent on chronic constipation / fecaloma. The discomfort can be eradicated through the specific intake of laxatives. The most used drug for this purpose is lactulose, an extremely delicate osmotic laxative active ingredient, capable of drawing water into the intestinal lumen, softening the stool and stimulating intestinal peristalsis. Even suppositories of glycerin or bisacodyl (eg Dulcolax) can be beneficial in the presence of faecal incontinence related to constipation.
- Case 2: fecal incontinence dependent on chronic diarrhea. The disorder must clearly be treated with antidiarrheal drugs:
- The Loperamide principle (eg Imodium) is particularly suitable for relieving diarrhea, thereby improving the disturbance of fecal incontinence. Loperamide increases the tone of the anal sphincter, while reducing bowel movements (peristaltic contractions) and the frequency of bowel movements.
- Anticholinergics (eg Atropine, Belladonna): indicated for reducing intestinal secretions and regulating the movements of the viscera.
- Opioids (eg codeine): in addition to the treatment of cough, some opioids such as codeine are used as intestinal motility inhibitors. However, it should be noted that these drugs, compared to the previous ones, are much less used for the treatment of fecal incontinence due to the important side effects related to them.
- Activated carbon: active ingredient indicated to reduce the water content in faeces.
Alternative interventions
For all those cases of partial fecal incontinence (of minor entity), a new therapeutic-rehabilitative method has been developed - known as tactile biofeedback - very useful for detecting the subject's sphincter activity. This is an intervention strategy indicated for patients who experience a reduction in rectal sensitivity, but who still have marked sphincter activity. Biofeedback is a special rehabilitation technique aimed at strengthening the pelvic floor muscles: here, the patient is "educated" to contract and release the muscles in the anal site in order to resist the urge to defecate at inopportune moments (for further information: read Kegel exercises).
The biofeedback treatment, always performed on an outpatient basis, involves the introduction of a small probe into the anal canal and into a part of the patient's rectal ampulla. This probe, which records the pressures exerted on the walls of the anal canal, is connected to a computer that processes the data and transforms them into pulses and colored bars. The different colors of the bars indicate the degree of contraction and relaxation of the affected muscles. After obtaining the right indications from the doctor on the correct way to perform the pelvic floor exercises, the patient himself will evaluate how he performs them by observing and studying the colored bands recorded by the monitor.
It is not uncommon that, as a support to biofeedback, the patient is also subjected to passive gymnastics, known as electrotherapy: this treatment consists of stimulating the fibers of the anal muscles by inserting an electrode into the anal canal. The benefits derived from electrotherapy are however uncertain; therefore its implementation is not always justified.
Some patients suffering from fecal incontinence may benefit from the application of so-called anal swabs: these are real plugs that are inserted into the anus to hinder the involuntary loss of fecal material.
Surgical interventions
When neither drug action nor rehabilitation strategies are sufficient to combat fecal incontinence, the patient is forced to undergo surgery. Most often, surgery is needed when fecal incontinence is related to rectal prolapse or childbirth injuries. Based on the triggering cause, the most performed surgical treatments include:
- Surgical correction of rectal prolapse, hemorrhoids, rectocele
- Sphincteroplasty: indicated to repair an anal sphincter where there is a traumatic lesion of the muscles involved in defecation.
- Restoration of muscle tone of the anal sphincter (gracileplasty): in some cases, it is possible to repair the anal sphincter by wrapping a muscle taken from the patient's thigh over it. The very delicate method consists precisely in the transposition with electrostimulation of the gracilis muscle (adductor muscle that occupies the medial portion of the thigh) to the anus.
- Artificial anal sphincter: surgery indicated for severe cases of fecal incontinence related to damage to the anal sphincter. A sort of inflatable ring is implanted in the anal canal to control the loss of fecal material. When swollen, the device prevents the anal sphincter from releasing (therefore there is no loss of stool); vice versa, when you want to defecate, it is possible to deflate this special ring by means of an external pump, thus activating normal intestinal activity.
- Colostomy: it is undoubtedly a drastic surgical choice, performed as a last resort for the patient suffering from a severe form of fecal incontinence. During this surgery, a new artificial communication is created that connects the colon with the abdominal wall through an opening in the abdomen. A special pouch is attached to this opening to collect the fecal material.
Diet
Changes in eating habits can undoubtedly improve the faecal incontinence disorder considerably (and even prevent it from returning). The first precaution is the total elimination of alcohol and the limitation of caffeine in the diet: when taken in excess, these two substances (alcohol and caffeine) can in fact induce diarrhea and fecal incontinence.
When the defecation disorder is strictly related to diarrhea, the patient should prefer foods that can compact the intestinal material. To this end, the recommendation is to increase the amount of dietary fiber - for example from bran and whole foods - and to limit the intake of all those foods capable of inducing a laxative effect. Spices, spicy foods, smoked foods, artificial sweeteners should also be avoided or at least limited in patients prone to diarrhea (see: diet and diarrhea).
Some lactose intolerant people tend to develop not only diarrhea but also fecal incontinence: for this reason, eliminating foods containing this sugar from the diet is an important dietary measure to prevent diarrhea and fecal incontinence.
Patients suffering from chronic constipation should instead pay particular attention to the correct intake of both fibers and liquids (drink at least 2 liters of water a day), two essential components for softening the intestinal contents, facilitating evacuation, thus preventing incontinence. fecal.
Other articles on 'Faecal incontinence: treatment, interventions and diet'
- Faecal incontinence: symptoms, complications and diagnosis
- Faecal incontinence