«Diet As a Cause of Hepatitis
After having illustrated the role of nutrition as a possible cause of various types of hepatitis, let's try to understand what are the objectives of a diet aimed at treating liver disease.
 Both in the case of acute hepatitis and chronic hepatitis, the diet aims to: REDUCE fatigue of the organ, COMPENSATE any lack of its metabolic functions, ELIMINATE the predisposing causes (if dietary) and PREVENT a worsening of the organ pathology.
Both in the case of acute hepatitis and chronic hepatitis, the diet aims to: REDUCE fatigue of the organ, COMPENSATE any lack of its metabolic functions, ELIMINATE the predisposing causes (if dietary) and PREVENT a worsening of the organ pathology.
Strange as it may seem, in many cases it is NOT possible to pursue all the above objectives at the same time; a choice between the various possibilities is therefore necessary. This decision (ALWAYS and ONLY at the DISCRETION of the TREATMENT SPECIALIST DOCTOR) must be made according to some primary factors, which are: severity of hepatitis, organ function and failure, other comorbidities, prognosis and subjective characteristics of the patient, etc. definitive, there is NOT ONLY ONE diet for hepatitis, as this must be established according to the situation; it is therefore no coincidence that various diets for hepatitis can also be almost diametrically opposed to each other. Furthermore, although they are potentially (but not necessarily!) Related, it is necessary to specify that "hepatitis" and: LIVER INSUFFICIENCY, HEPATIC FIBROSIS, LIVER CIRRHOSIS or LIVER CARCINOMA NO are synonyms! It is in fact possible that severe acute hepatitis causes transient but treatable liver failure, or that chronic hepatitis does not induce liver failure but tends to slowly evolve into fibrosis and then into cirrhosis; again, it is possible that a steatohepatitis rapidly passes to a mild but stable cirrhotic state. In short, the possibilities are really many!
In any case, among all this necessary variability, there are some UNIVOCALLY shareable rules, which are:
- ABOLITION of ALCOHOL
- ABOLITION of DRUGS and food SUPPLEMENTS NOT NECESSARY
- ABOLITION / REDUCTION to the minimum terms of OTHER NERVINS (coffee, tea, chocolate ...) and of SALT (and, if desired, also of SUGAR) ADDED
- ABOLITION of Junk or FAT FOOD or in any case rich in REFINED SUGARS
- REGULARIZATION of meals and TREND to NUTRITIONAL BALANCE (FORBIDDEN both FASTING and EXCESS CALORIES, especially if over 10% of the NORMALcaloric).
WARNING! The article refers to the DIET intended as FOOD nutrition for hepatitis, therefore it excludes ENTERAL and PARENTERAL nutrition! Obviously, in the case of severe hepatitis (or in any case in the midst of acute symptoms), the use of parenteral medicine is more usual; however, in the long periods of artificial nutrition, the use of enteral nutrition is increasingly indicated, which guarantees the maintenance of the functionality of the various digestive organs.
First, we will analyze the diet for alcoholic and / or food steatohepatitis; then, the diet for hepatitis WITHOUT severe impairment of liver function will be described. Finally, we will mention the basic nutritional principles for hepatic degeneration and the complications to which it is associated (ascites, encephalopathy, portal hypertension, haemorrhages, etc.).
Diet for Alcoholic and / or Alimentary SteatoHepatitis - Diet for Fatty Liver
Steatohepatitis is the most common liver disorder in the populations of industrialized countries.
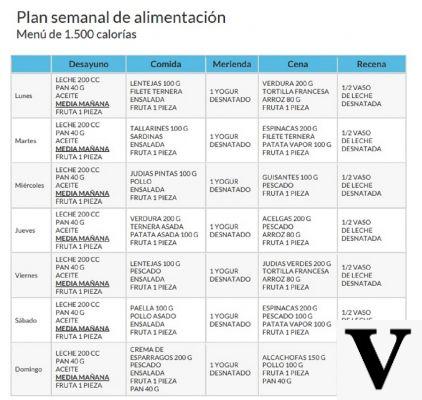
The diet for this hepatitis (which can be acute or chronic depending on the case) is, to be honest, very simple. First, it is FUNDAMENTAL to remove the etiological origin of steatosis, i.e. alcohol abuse on the one hand and food abuse on the other (possibly both!). Then, since it is a condition frequently linked to overweight / obesity, the diet should be associated with a program of physical motor activity and acquire a certain slimming effect; Ultimately, the fatty steatosis diet is often a low-calorie diet which subtracts 30% of the total energy needed to maintain normal weight.
The nutritional organization is quite rigid, especially as regards the absence of alcohol, sweet foods and junk foods. The abolition of added sucrose (and of the foods that contain it), and of cooking salt (as well as of the foods that include it) is required. The main lipid source is extra virgin olive oil, the protein one is mixed, therefore composed of animal and vegetable foods, while simple sugars are ONLY contained in vegetables in raw form and in dairy products (fruit, vegetables, semi-skimmed milk and natural yogurt). All cereals are whole and possibly whole (not in the form of flours and derivatives); however, these must be alternated with legumes, obtaining a grain-legume ratio of 2: 1 or even 1: 1. The vegetables, to be eaten in alternating raw and cooked form, are in season and in portions ranging between 100 and 200g for both lunch and dinner. Fruit and yogurt alternately structure secondary meals.
The breakdown in energy nutrients is balanced, that is: about 1g / kg of DESIRABLE PHYSIOLOGICAL weight in proteins, 25% of lipids with the greatest possible amount of unsaturated (omega3 / omega6 ratio 1: 4 - omega 9 in abundance), and the rest energy in totally complex carbohydrates, with the exception of fructose and lactose in food. Respecting individual susceptibility, the fiber must reach 30g / day and both the mineral salts and the vitamins must comply with the right recommended rations. Meals must be at least 5 and with the same caloric breakdown of a balanced diet: 15% for breakfast, 5-10% for the two snacks, 35-40% for lunch and 30-35% for dinner.
In restoring hepatic integrity, all the plant molecules with a phyto-therapeutic action (therefore antioxidant, hypocholesterolemic, hepatoprotective, etc.) acquire a very important role; among these: vegetable lecithins, phytosterols, phenolic substances, etc. In particular, the phenolic substances must be abundant, perhaps with a good content of cynarin (ie a polyphenol contained in artichokes) and silymarin (a phenolic complex abundantly contained in milk thistle). Even the intake of provitamin A, vit. C and vit. And it promotes the improvement of the liver condition (especially C).
In the case of alcoholic steatosis, since alcoholism causes intestinal malabsorption and the reduction of vitamin stocks (if any!), The subject could significantly benefit from generic food supplementation and above all from thiamine (vitamin B1).
Diet for Hepatitis Without Serious Impairment of Liver Function
After the previous one, the diet for hepatitis without severe impairment is certainly the most used. It includes all forms of acute or chronic infectious / parasitic hepatitis. It has enormous application in the treatment of chronic HBV virus hepatitis (which affects about 350.000.000 people in the world) and has many aspects in common with that already described.
Compared to the diet for food or alcoholic fatty steatohepatitis, this does not require you to "empty" the liver cells of excess fat and glycogen. It goes without saying that, albeit desirable, motor activity fades into the background or is totally abolished in acute forms and, except for the presence of other comorbidities, the same applies to slimming capacity.
On the other hand, some precautions already mentioned are much more important, such as the abolition of alcohol, unnecessary drugs and supplements, and the absolute moderation of other nerves, salt, sugar and junk foods. Furthermore, despite what one might believe, it is essential to AVOID fasting or excessive calorie REDUCTION, as well as overeating and excess energy.
The liver is the organ responsible for many metabolic functions, including gluconeogenesis, lipogenesis and proteosynthesis; but also to the production of digestive bile. By virtue of the fact that, in the case of hepatitis, it is necessary to reduce the organ's "workload" as much as possible (for blood homeostasis and digestion), the diet must necessarily be NORMALcaloric. Fasting or an insufficient diet REQUIRE a greater hepatic effort than normal, since the organ must produce glucose (essential for the central nervous system) from glycerol and circulating amino acids. Furthermore, we remind you that prolonged hypo-nutrition (and above all carbohydrate depletion) determines the accumulation of ketone bodies, potentially TOXIC molecules for all tissues. Not least, an insufficient diet DOES NOT allow the supply of essential amino acids in sufficient quantities for protein synthesis; the liver, already less efficient because it is sick, if it is not supplied with these substrates, finds it difficult to produce all the protein molecules of the plasma. On the other hand, an energy surplus involves other drawbacks; first of all, hepatocytes must increase biliary production for the emulsion of fats in digestion. Secondly, excess amino acids and carbohydrates in the diet require conversion to fatty acids by the liver; here, again, there is an increase in the total WORK of the organ (without considering the possible tendency to fatty steatosis).
It is then necessary to make a final clarification on the relevance or otherwise of other molecules in the diet. In my opinion, in the nutritional regimen for hepatitis, it is also strongly advisable to significantly limit the concentration of certain additives (especially sweeteners and preservatives). We reiterate for the umpteenth time that the liver is responsible for the metabolization of most of the nutritional and circulating molecules in the blood, which is why it is conceivable that the excess of these synthetic products requires a greater effort on the part of the organ.
Finally, I focus on a generally unknown but far from negligible detail, namely the use of fructose as a sweetener. It must be clear that I am not talking about fructose NATURALLY present in foods (fruit and vegetables), but about the granular one. This, which is not well oxidizable by human cells, must necessarily be converted by the liver into glucose. While that naturally introduced with raw foods reaches percentages ranging from 10 to 16% of total calories, using sweetened foods, sweetening drinks and granular fructose for seasoning, this value can even double.
The breakdown of macronutrients is the same as in the previous diet, as is the energy breakdown of meals. Again good amounts of antioxidants and dietary supplementation with vitamins can be of great help.
Notes on the Nutritional Needs of Hepatic Insufficiency
Hepatic insufficiency can be mild, moderate or severe, and also present itself (in conjunction with hepatitis) in an acute or chronic form. It is necessary to take into account, first of all, that hepatic insufficiency is characterized by a reduction in organ functions.
In mild forms, frequently supported by traditional nutrition and not by artificial nutrition, it is advisable to use easily digestible meals, with moderate portions, but without neglecting the overall nutritional intake.
On the other hand, starting from the moderate form and ending with the severe one (often subject to enteral or parenteral nutrition) the following precautions are required:
- Salt exclusion from the diet, to reduce the tendency to edema and ascites
- Moderation of the MA protein quota with a supplement of branched amino acids, since they do not require hepatic metabolization before cellular oxidation and have a very low level of nitrogenous waste (in turn responsible for the onset of hepatic encephalopathy). It is not possible to reduce too much the intake of amino acids as it would further alter the proteosynthesis of the liver; the consequent reduction of plasma proteins would determine: the collapse of oncotic pressure with a tendency to edema and ascites, and less coagulation capacity with the risk of bleeding
- Some authors suggest structuring a diet richer in energy than the normal one, that is, a HIGH-calorie diet. Personally I do not contest the choice but it is certainly necessary that these extra calories are mainly provided by glucose.