prostate
The prostate is an organ that is part of the male reproductive system; more precisely, it is an exocrine gland which, with its secretion, participates in the composition of the seminal plasma, which is the support substrate and vehicle for spermatozoa.
The spermatozoa and seminal plasma (also enriched by the secretion of the seminal vesicles and epididymis) form the sperm, which is introduced into the urethra and ejaculated outwards during coitus.
The prostate is an organ rather susceptible to aging of the organism. Among the pathologies / disorders that affect it most frequently we remember: prostatitis (or inflammation of various kinds of the prostate), prostatic hypertrophy and prostate cancer. Unlike the last two, prostatitis is NOT typical of aging.
Classification
Prostatitis, or inflammation of the prostate gland, can have different etiological causes; the most frequent are of INFECTIOUS origin and occur mainly in adults and the elderly, especially if catheterized.
The causes of prostatitis infectious are: sexual contagion (due to pathogens rising from the urethra), reflux of infected urine (caused by concomitant pathological changes in the urethra, bladder or prostate itself), direct or lymphatic infection from the last intestinal tract (due to severe constipation or colic infections) and blood vehicle (originating from infections of other districts).
Le NON-infectious prostatitis they are called abacterial or prostatosis. The most common causes are: stagnation of blood and accumulation of secretion (due to congestion due to prolonged sexual stimulation without release, interrupted coitus, long abstinences, etc.), repeated microtrauma (cycling), severe constipation and hemorrhoids.NB. Prostatosis also includes forms of infectious prostatitis with an unidentifiable bacterial load. Those secondary to severe constipation and / or hemorrhoids can contribute to the so-called "chronic pelvic pain syndrome".
A last form of inflammatory prostatitis is usually diagnosed randomly during other diagnostic tests and, since it does not appear to manifest itself in any way, is referred to as "asymptomatic".
Acute and Chronic
Pathogenic acute prostatitis is manifested by fever, generalized malaise, acute retention of urine, cloudy urine, peri-renal or lumbar pain, testicular pain, and disturbed urination. The treatment, in case of bacterial infection, is mainly constituted by the timely administration of broad-spectrum antibiotics and possibly analgesic anti-inflammatory drugs. Proper diet can be of great help.
Chronic prostatitis manifests itself with pain, often fever (but only in the case of the infectious one), a sense of heaviness in the peri-renal area, urethral pain, sometimes urination disturbances. Chronic prostatitis is more difficult to cure; if present, it is necessary to identify the responsible pathogen in order to identify a specific antibiotic.
In the event that it is not possible to identify the specific pathogen (as in chronic pelvic pain syndrome), the symptoms, predisposing factors and any complications are reduced. Also in this case, but for different reasons, a correct diet can be helpful or even decisive.
Diet
Diet for prostatitis can be a valuable contribution:
- To the moderation of symptoms for acute infectious or chronic infectious forms
- To the treatment for secondary non-pathogenic ones (linked to blood circulation disorders due to colorectal pain or food-borne irritants).
First, let's remember that the diet for prostatitis is NORMALcaloric, that is, it tends to maintain the physiological weight of the subject; in the event that the person also suffers from overweight, the normocaloric diet for prostatitis "could" determine a more or less significant reduction in adipose tissue.
For both acute and chronic, infectious or non-pathogenic, the diet for prostatitis is ALWAYS rich in liquids and essentially made up of light foods, easy to digest, little processed, with few FAT ingredients of animal origin, and rich instead of lean products rich in water.
The diet for non-pathogenic prostatitis and secondary to other intestinal disorders is AIMED at the resolution of the triggering agent. In this case (especially in chronic pelvic pain syndrome), they become diets for prostatitis: the irritable bowel syndrome diet, the constipation diet and the hemorrhoid diet.
These three types of diets are extremely similar, except in the forms of irritable bowel which also manifest bouts of diarrhea. These diets are therefore real nutritional therapies and have the objectives of:
- Minimize irritation of the colic mucosa
- Increase the frequency and ease of bowel movements
- Prevent and possibly reduce the symptoms of hemorrhoids
All this is absolutely NECESSARY to combat the "potential" triggering factor of certain prostatitis, or the alteration of the circulatory flow DUE to the well-known haemorrhoidal disease. In fact, due to the swelling and inflammation of the haemorrhoidal vessels (haemorrhoids), the blood stream badly irrigates the prostate gland, causing specific symptoms; moreover, the excessive expansion of the colon adjacent to the prostate, in addition to causing poorly identifiable pelvic pain, can cause compression of the gland and cause further discomfort.
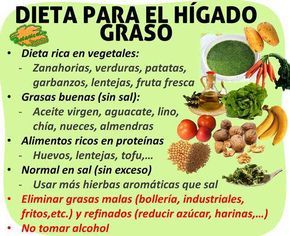
From a nutritional point of view, to combat colic irritation, constipation and hemorrhoids, the diet for prostatitis aims to:
- Increase the intake of dietary fiber, possibly with "bulk" laxatives
- Increase your water intake
- In some cases, increase the intake of lipids (better unsaturated)
NB. total fats must never exceed 30% of calories, to avoid the risk of fatty deposits and digestive difficulties - Decrease the nerves: alcohol, caffeine, etc.
- Reduce dietary waste: charred macronutrients in cooking
- Decrease irritants such as pepper, many spices or capsaicin
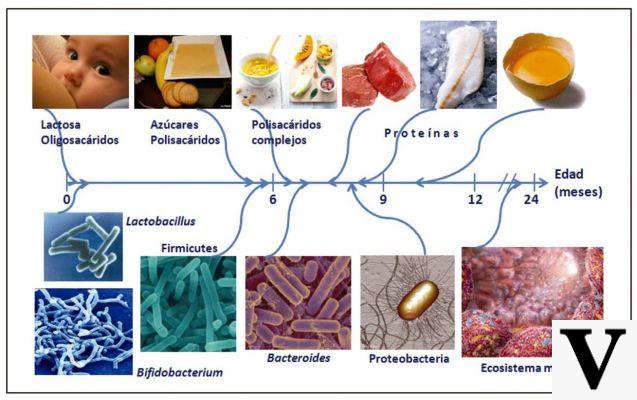
- Promote the development of physiological bacterial flora in the large intestine
In practice, as regards the choice of alimony, in the diet for prostatitis it will be necessary:
- Drink at least 1,0 ml of water for every 1,0 kcal consumed in the diet
- Increase whole grains and legumes (the latter, even without peel)
- Above all, increase vegetables and also fresh fruit
- Increase soupy recipes at the expense of dry ones
- Prefer cold-pressed and raw oils as a condiment
- Eliminate all alcoholic beverages, coffee, tea (especially black), chocolate and energy drinks
- Discard the hot spices
- Eliminate all the intense and fast cooking systems, but do not use the extra cooking too much; prefer boiling and steaming
- Eliminate smoking
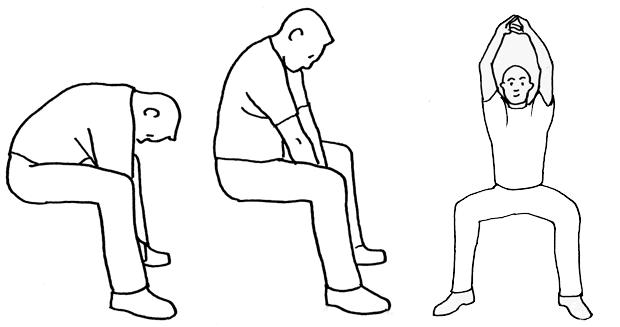
- Practice regular physical activity.
In conclusion, the diet for prostatitis varies according to the pathological cause of the specific prostatitis and, in case it is related to intestinal disorders, the nutritional regimen can also contribute to the resolution of the disorder.