Hepatitis C
Hepatitis C is an infectious disease caused by the HCV virus, which primarily affects the liver.
In the initial period of infection, symptoms are absent or barely noticeable; fever, dark urine, abdominal pain and jaundice rarely occur.
Few manage to recover completely and most of the subjects become chronic.
Over the years, chronic hepatitis C can induce liver disease - such as cirrhosis, fibrosis, functional failure and cancer - and / or esophageal and gastric varices.
Diagnosis is made with blood tests.
Hepatitis C is mainly spread through blood-to-blood contact (intravenous use of drugs, medical equipment, childbirth, wounds, and transfusions), NOT by casual contact (hugging, kissing, sharing tableware, food, and water) .
There is no vaccine for hepatitis C and chronic infection can be cured with drug therapy; those who have developed liver cancer or cirrhosis may require a transplant (not always decisive).
Worldwide, approximately 130-200 million people are infected with hepatitis C (mainly in Africa and Asia).
Diet and Motor Activity
Since there is no form of food contagion, the hepatitis C diet does not play a major role in preventing the disease.
On the other hand, we have already highlighted that, in the long term, hepatitis C is capable of causing cirrhosis, fibrosis and finally cancer; obviously, these conditions are associated first with a reduction in function and then with overt liver failure.
The diet for liver failure is not the same as that designed to treat a suffering liver. Below we will talk above all about how to deal with an intermediate situation, which does NOT provide for the diagnosis of liver failure proper.
Obviously, a liver unable to fulfill its numerous tasks (oncotic pressure, synthesis of transport proteins, production of digestive bile, glycemic homeostasis, pharmacological metabolism, etc.) significantly compromises the general state of health.
When chronic hepatitis C affects liver function, it becomes necessary to reduce the overall metabolic effort.
Among the various processes that are influenced by diet and lifestyle we recognize: proteosynthesis, proteolysis, transamination, glycogenosynthesis, glycogenolysis, lipogenesis, lipolysis, pharmacological and hormonal metabolism, bile production, etc. To do this, first of all you need to:
- Structuring a balanced diet, normocaloric and well distributed between meals
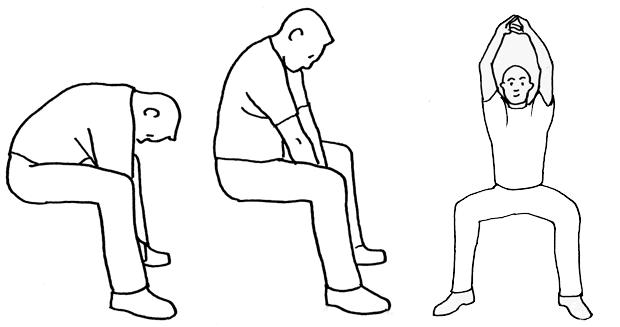
- Avoid a sedentary lifestyle, as well as intense motor activity
- Avoid unnecessary medications and supplements.
Liver failure and diet
When the reduction in hepatic functional capacity is very high (as occurs, for example, in decompensated cirrhosis), the nutritional needs become totally different and variable according to the type of complications manifested (portal hypertension, encephalopathy, ascites, renal impairment, coagulation etc.).
First of all, the subject must be put at absolute rest, possibly in a lying position, to promote venous return. Often, at this point, the patient requires injecting nutrition.
In case of encephalopathy, it is absolutely necessary to reduce the total protein intake by up to 50%, estimating it at approximately 0,5g of peptides per kilogram of body weight.
Keep in mind that liver failure also causes a decrease in the protein synthesis of blood factors (coagulation, transport proteins, etc.). For this reason, in the absence of encephalopathy, the protein quantity in the diet (necessary for the synthesis of the aforementioned proteins) must NOT be absolutely reduced (1,2 and up to 1,5g / kg); the risk would be to aggravate this functional incapacity.
Furthermore, from recent studies it seems that it is advisable to replace aromatic amino acids with branched ones, which DO NOT have an equally negative impact on azotemia.
At the onset of ascites, however, it is recommended to carry out a severe restriction of sodium (contained in table salt and, to a lesser extent, in natural foods), bearing in mind that excluding it completely could worsen the functionality of already compromised kidneys. .
Nutritional Principles
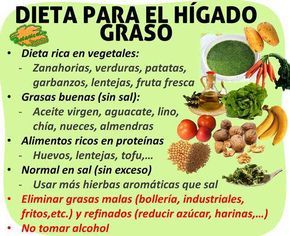
The essential nutritional principles for maintaining satisfactory liver function in the presence of chronic hepatitis C can be summarized as follows:
- Abolish ethyl alcohol and all nerves. Alcohol acts negatively on liver cells and worsens the metabolism of vitamin B1 (which the liver is not able to store anyway); nerves, on the other hand, are totally useless molecules that the liver must metabolize before being expelled in the urine by the kidneys.
- Abolish junk or unhealthy foods and drinks. This group includes all fast-foods (french fries, croquettes, pancakes, hamburgers, etc.), industrial sweet and savory snacks and sweet drinks (carbonated or not).
Junk foods have a nutritional profile characterized by the richness of harmful molecules; some of these are: saturated or hydrogenated fats (also in trans conformation), refined sugars (sucrose, maltose, added granular fructose), food additives (dyes, flavor enhancers, preservatives, sweeteners, etc.) and toxins released in cooking techniques such as high intensity (by irradiation or metallic conduction) such as: acrylamide, formaldehyde, acrolein, polycyclic aromatic hydrocarbons, etc. - Encourage the consumption of fresh (possibly frozen) or raw foods, limiting those that are processed and / or refined. Various processes, for example the process of pearling the seeds or the whitening of the flours - but also the mixing of meat / fish with other ingredients to create sausages or croquettes or other doughs (such as surimi) - exploit chemical and physical mechanisms that deprive the food of many useful nutrients. Suffice it to say that, in refined flours, the overall nutritional reduction of fibers, salts, vitamins and essential fats is close to 80%. In particular, in the diet for hepatitis C there must be absolutely no lack of coenzymatic vitamin factors, necessary to support many cellular processes of the specific tissue; although the liver is known to be a very effective vitamin reserve, due to the infection it could lose (at least in part) this capacity.
- Structuring a normal calorie regime. This means that the energy intake must be sufficient to maintain weight, without it increasing or decreasing, circumstances in which the organ has to perform a greater amount of work.
- For the same reason, it is important that energy is divided into at least 5 meals, 3 of which are main and 2 are secondary. A solution may be recommended that includes: 15% of calories for breakfast, 7-8% for mid-morning and mid-afternoon snacks, 35-40% for lunch and dinner.
- Maintain nutritional balance. This could be summarized as follows: lipids 25-30% of calories, proteins about 0,8-1,5g / kg and all the rest in carbohydrates (of which, not more than 10-16% simple). The contributions of fiber, mineral salts, vitamins and cholesterol must also fall within the limits of specific needs. In addition, non-vitamin or saline antioxidants, such as phenolic ones (contained mainly in fruit and vegetables), must not be missing. To get a better idea of how a similar nutritional regimen could be organized, it is advisable to read the article: Eat Healthy.
- If the subject is gluten intolerant, the hepatitis C diet must exclude: wheat, spelled, spelled, rye, barley, oats and sorghum. In fact, decompensated celiac disease is responsible for an increase in systemic inflammation and abnormal immune activation. In place of the above cereals, it is possible to choose: millet, rice, corn and teff, or pseudocereals such as quinoa and amaranth, or even all legumes (beans, lentils, peas, broad beans, lupins, chickpeas, etc.). NB. It is better to avoid grass peas, especially in large quantities, due to their (toxic) oxalylldiaminopropionic acid content.
- It is absolutely forbidden to drink non-potable water and take food or drinks potentially contaminated by them. In the case of hepatitis C, the liver is unable to optimally metabolize any chemical or other toxic residues.
- Plenty of fresh fruit and vegetables. The foods that belong to the VI and VII fundamental groups of foods are the main sources of vitamin C, carotenoids (provitamin A), vitamin K and various types of antioxidants (such as phenolics). In all, it would be advisable to provide 4-5 portions of fresh fruit and vegetables of 150-300g each, preferably mainly raw.
- Promote the intake of therapeutic nutrients for the liver. In addition to the various antioxidant factors (some of which also have anti-inflammatory, anti-tumor power, etc.) it is quite useful to increase the phytoelements that exert a hepato-protective role; for example, cynarin and silymarin from artichoke and milk thistle.
- Emphasize the contribution of polyunsaturated fatty acids to the detriment of saturated ones, both in proportion and in quantitative terms. It is particularly advisable to increase the dietary content of omega 3 essential fatty acids and not too much that of omega 6.
Omega 3 (ALA, EPA and DHA - see article: Omega 3 and Omega 6 Fatty Acids) are anti-inflammatory precursors and can help the body reduce general inflammation; arachidonic acid (a derivative of omega 6), on the other hand, has the opposite effect. The most suitable foods are: blue fish (mackerel, mackerel, bonito, anchovies, sardines, etc.), some oil seeds (almonds, sesame, etc.) and some cold-pressed vegetable oils (extra virgin olive oil, linseed, walnut etc).
Other articles on 'Diet and Hepatitis C'
- Medicines to Treat Hepatitis C
- Hepatitis C
- Hepatitis C: risk factors, diagnosis and prevention
- Hepatitis C: care and treatment